Dysplastic Cerebellar Gangliocytoma Free
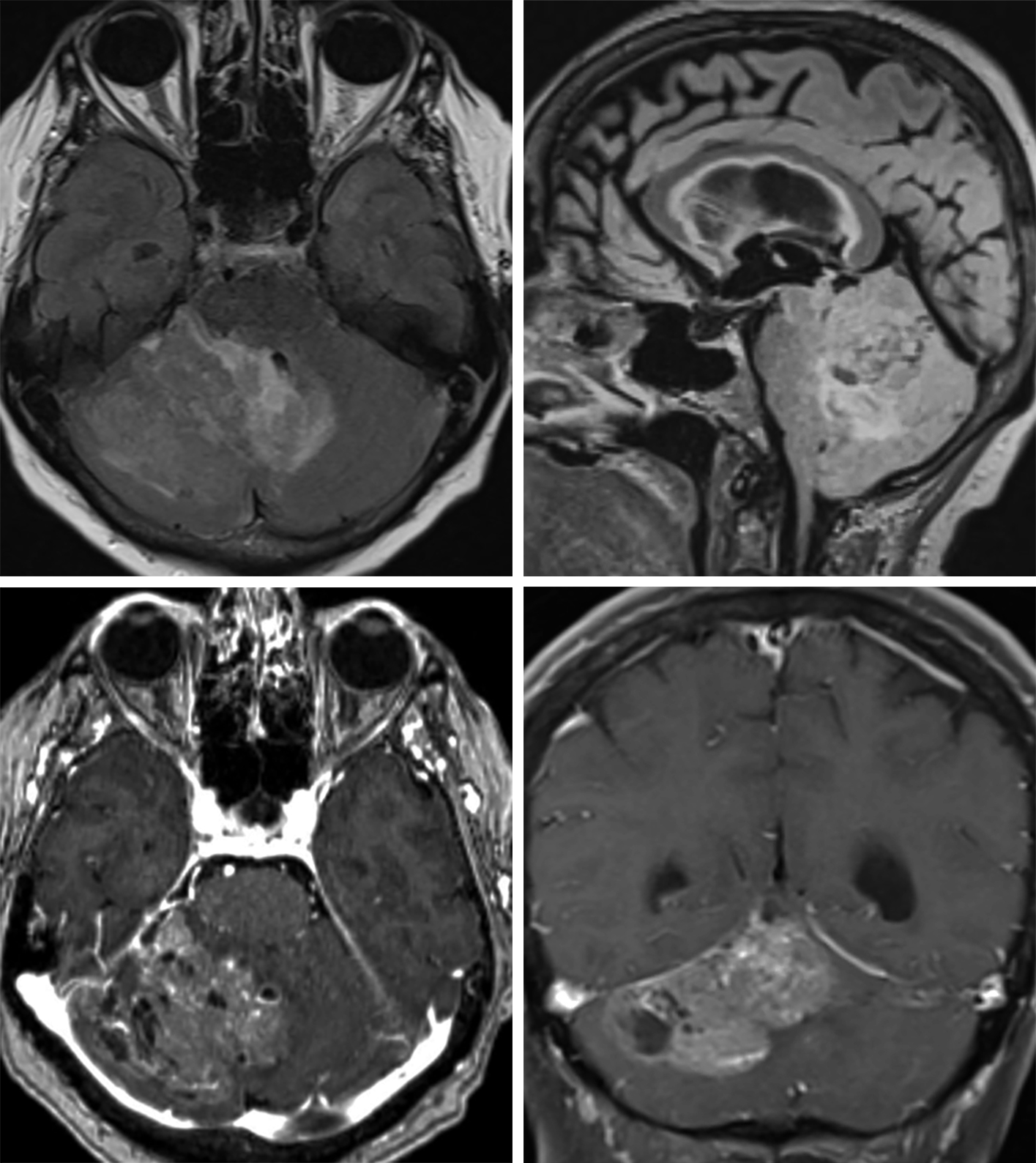
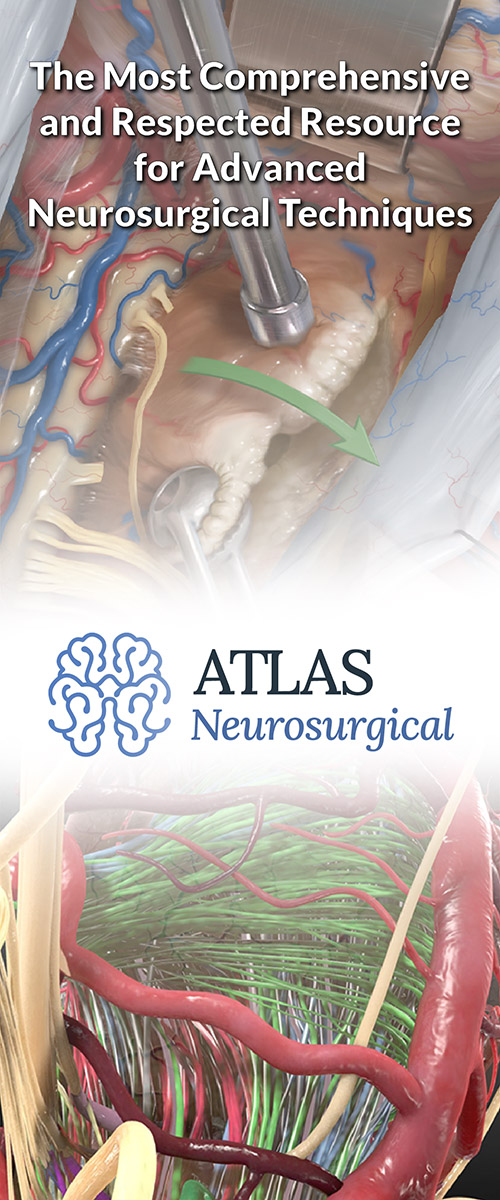
Figure 1: (Top Left) A disorganized appearance to the cerebellum is typical in this dysplastic cerebellar gangliocytoma, barely visible on T1WI. (Top Right) These lesions are often associated with variable degrees of T2 hyperintensity and enhancement. (Bottom) This patient's lesion demonstrated no enhancement on T1WI postcontrast imaging.
Figure 2: This heterogeneous infiltrative lesion centered in the right cerebellar hemisphere on FLAIR (top left, axial; top right, sagittal) demonstrates only mild associated edema and mild mass effect for the size of the lesion. There are small cystic changes and conspicuous enhancing vessels, and single hemispheric dominance but midline crossing that are typical of dysplastic cerebellar gangliocytoma/L’hermitte-Duclos disease on contrast-enhanced imaging (bottom left, axial; bottom right, coronal). The degree of enhancement is moderate in this patient but highly variable in this type of tumor.
BASIC DESCRIPTION
- Also known as L'hermitte-Duclos disease (LDD), the neurologic manifestation of multiple hamartoma and neoplasia syndrome (MHAM) or Cowden syndrome (CS)
- CS + LDD = MHAM + LDD = COLD (Cowden-L'hermitte-Duclos syndrome), a neurocutaneous syndrome
- Benign cerebellar lesion of uncertain etiology
PATHOLOGY
- Benign cerebellar mass with thickened, irregular cerebellar folia
- Pathogenesis unclear: hamartomatous, neoplastic, or congenital
- WHO grade 1
- No malignant potential
- MHAM
- Autosomal dominant inheritance of PTEN mutation
- Hamartomas of skin, gastrointestinal and genitourinary tracts, mucosa, eye, and central nervous system
- Increased risk of mucocutaneous tumors, thyroid adenomas, fibrocystic breast disease, and polyps
- Absence of cerebellar Purkinje cells, abnormal ganglion cells, and hypertrophic granule cell layer are microscopic features
CLINICAL FEATURES
- Any age (20–40 years old at presentation most common)
- No gender predilection
- Common presenting signs/symptoms
- Increased intracranial pressure: headache, nausea, vomiting
- Cerebellar signs: ataxia, dysmetria, gait instability
- ±Clinical findings of MHAM/CS
- Treatment: surgical debulking ± CSF shunting
IMAGING FEATURES
- General
- “Corduroy,” striated, or tigroid appearance of cerebellar hemisphere due to thickened, irregular folia
- Most commonly unilateral cerebellar hemisphere involvement ± vermis
- Variable size
- Mass effect, tonsillar herniation, and hydrocephalus if large
- Stable size or slow growth
- CT
- Isodense to hyperdense lesion with thickened, irregular, and tigroid cerebellar folia
- Variable enhancement on contrast-enhanced CT
- MRI
- T1WI: hypointense to isointense
- T2WI: hyperintense with hypointense to isointense cerebellar folia; hypointense vascular flow voids
- DWI: hyperintense signal, which may represent “T2-shinethrough,” hypercellularity, or increased density of axons
- T1WI+C: variable enhancement
- MRS/MR perfusion: decreased NAA, Cho, and MI; increased relative cerebral blood volume (rCBV) and relative cerebral blood flow (rCBF) may be present
IMAGING RECOMMENDATIONS
- MRI without and with intravenous contrast including DWI and MR spectroscopy; evaluate for MHAM/CS if findings of LDD are present (and vice versa) due to increased risk of other malignancy
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Abel TW, Baker SJ, Fraser MM, et al. Lhermitte-Duclos disease: a report of 31 cases with immunohistochemical analysis of the PTEN/AKT/mTOR pathway. J Neuropathol Exp Neurol 2005;64:341–349. doi.org/10.1093/jnen/64.4.341.
Awwad EE, Levy E, Martin DS, et al. Atypical MR appearance of Lhermitte-Duclos disease with contrast enhancement. AJNR Am J Neuroradiol 1995;16:1719–1720.
Cianfoni A, Wintermark M, Piludu F, et al. Morphological and functional MR imaging of Lhermitte-Duclos disease with pathology correlate. J Neuroradiol 2008;35:297–300. doi.org/10.1016/j.neurad.2008.05.002.
Klisch J, Juengling F, Spreer J, et al. Lhermitte-Duclos disease: assessment with MR imaging, positron emission tomography, single-photon emission CT, and MR spectroscopy. AJNR Am J Neuroradiol 2001;22:824–830.
Murata J, Tada M, Sawamura Y, et al. Dysplastic gangliocytoma (Lhermitte-Duclos disease) associated with Cowden disease: report of a case and review of the literature for the genetic relationship between the two diseases. J Neurooncol 1999;41:129–136. doi.org/10.1023/a:1006167421100.
Osborn AG, Salzman K L, Jhaveri MD. Diagnostic Imaging (3rd ed). Elsevier, Philadelphia, PA; 2016.
Robinson S, Cohen AR. Cowden disease and Lhermitte-Duclos disease: characterization of a new phakomatosis. Neurosurgery 2000;46:371–383. doi.org/10.1097/00006123-200002000-00021.
Thomas B, Krishnamoorthy T, Radhakrishnan VV, et al. Advanced MR imaging in Lhermitte-Duclos disease: moving closer to pathology and pathophysiology. Neuroradiology 2007;49:733–738. doi.org/10.1007/s00234-007-0241-1.
Wei G, Liu S, Wu Y, et al. Teaching NeuroImages: MRI appearances of Lhermitte-Duclos disease. Neurology 2013;80:e67–e68. doi.org/10.1212/WNL.0b013e3182815454.
Please login to post a comment.