Pituitary Microadenoma
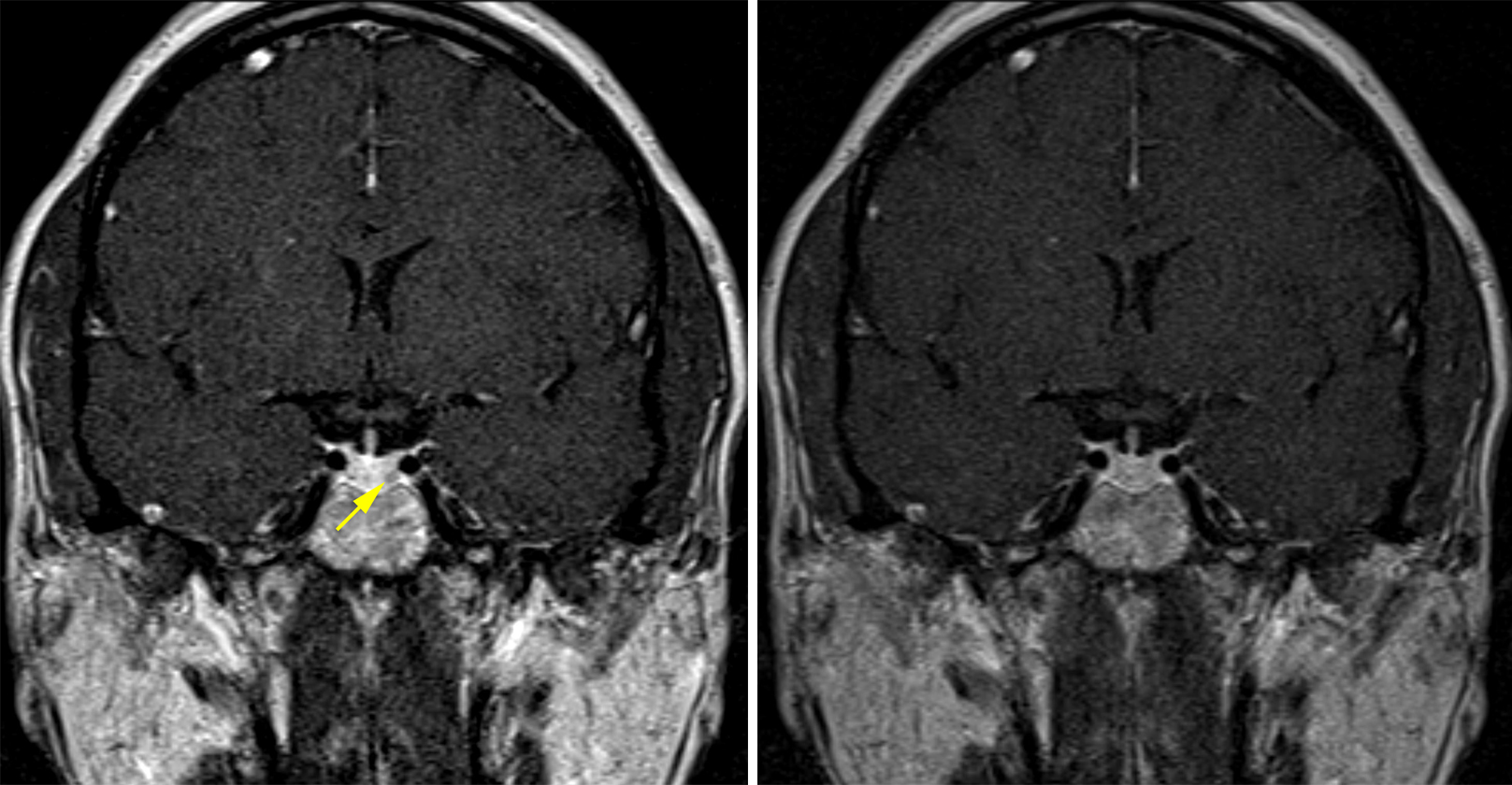
Figure 1: (Left) A tiny pituitary adenoma is visible on early postcontrast imaging as a nodule showing less enhancement than the surrounding pituitary tissue in the left inferolateral aspect of the pituitary gland (yellow arrow). (Right) This adenoma becomes invisible on the more delayed postcontrast imaging as the lesion and the pituitary gland become more similar in their degree of contrast enhancement.
BASIC DESCRIPTION
- Primary tumor of the adenohypophysis of various cell line differentiations, ≤10 mm in size
PATHOLOGY
- Low-grade tumors, WHO grade I
- Well differentiated, slow growing or nongrowing
- Can secrete hormones according to the cell of origin, most commonly prolactin
CLINICAL FEATURES
- Usually incidental (nonfunctioning)
- Can have symptoms related to hormone secretion (secretory)
- Prolactinoma is most common
- Women: irregular menses, amenorrhea, galactorrhea
- Men: hypogonadism, decreased libido
- Growth hormone secreting (acromegaly)
- Adrenocorticotropic hormone (ACTH) secreting (Cushing disease)
- Thyroid-stimulating hormone (TSH) secreting (hyperthyroidism)
- Prolactinoma is most common
- 10% of all patients on autopsy series
- More common in syndromes such as multiple endocrine neoplasia type 1 (MEN1) syndrome, McCune-Albright syndrome, Carney complex, familial isolated pituitary adenoma (FIPA) syndrome
- Pituitary apoplexy is a rare but serious complication
IMAGING
- General
- Small intrasellar mass, <10 mm in size
- Can be cystic, proteinaceous, or hemorrhagic
- Can demonstrate elevated contour on the superior margin of the affected side of the pituitary gland
- Can deviate the infundibulum away from the side of the microadenoma
- CT Imaging
- Usually not visible, nonrevealing
- Cystic or hemorrhagic lesions can be visible as tiny hypodense or hyperdense lesions
- Can see slight deviation of the infundibulum
- Thin-cut CT imaging might be helpful for delineating sphenoid sinus bony anatomy for surgical planning
- MRI
- T1WI: usually not visible unless cystic (hypointense) or hemorrhagic/proteinaceous (hyperintense)
- T2WI: variable, hyperintense if cystic
- FLAIR: variable, hyperintense if cystic
- DWI: usually not visible or obscured by adjacent sphenoid sinus/bone susceptibility artifact
- T1WI+C: usually enhances similar to surrounding pituitary gland on routine postcontrast imaging; on dynamic postcontrast images through the sella, microadenomas might be more visible at a time point during which they enhance less than normal pituitary tissue because of their comparatively delayed enhancement pattern
- Advanced imaging: these lesions are too small to appear on most advanced imaging modalities (MR spectroscopy, MR perfusion)
- Conventional Angiography
- Inferior petrosal sinus sampling (IPSS) is more accurate for identifying ACTH-secreting microadenomas than imaging alone
IMAGING RECOMMENDATIONS
- MRI without and with contrast with detailed images of the sella, including dynamic coronal postcontrast sequences
- Thin-cut CT imaging of the sinuses or sella can be helpful for delineating sphenoid sinus anatomy before transsphenoidal resection and during intraoperative navigation
For more information, please see the corresponding chapter in Radiopaedia.
Contributor: Rachel Seltman, MD
References
Aron DC, Tyrrell JB, Wilson CB. Pituitary tumors. Current concepts in diagnosis and management. West J Med 1995;162:340–352.
Chen CC, Carter BS, Wang R, et al. Congress of Neurological Surgeons systematic review and evidence-based guideline on preoperative imaging assessment of patients with suspected nonfunctioning pituitary adenomas. Neurosurgery 2016;79:E524–E526. doi.org/10.1227/NEU.0000000000001391.
Osborn AG. Osborn's Brain: Imaging, Pathology, and Anatomy. Amirsys, Salt Lake City, UT; 2013:699–705.
Raff H. Cushing syndrome: update on testing. Endocrinol Metab Clin North Am 2015;44:43–50. doi.org/10.1016/j.ecl.2014.10.005.
Vance M. Pituitary adenoma: a clinician's perspective. Endocr Pract 2008;14:757–763. doi.org/10.4158/EP.14.6.757.
Please login to post a comment.